WBCT on the Program Thursday, January 22 11:10 am – 12:30 pm Symposium 2: Diagnostic…
Surgeons Weigh In: Top Indications for WBCT: Part 3
Weight bearing CT (WBCT) imaging has fundamentally changed the evaluation and management of foot and ankle disorders such as hallux valgus, progressive collapsing foot disorder (PCFD), ankle instability, and traumatic deformities. The following panelists of experts share their insights and experiences in the use of WBCT in clinical practice as well as the future direction of the modality.
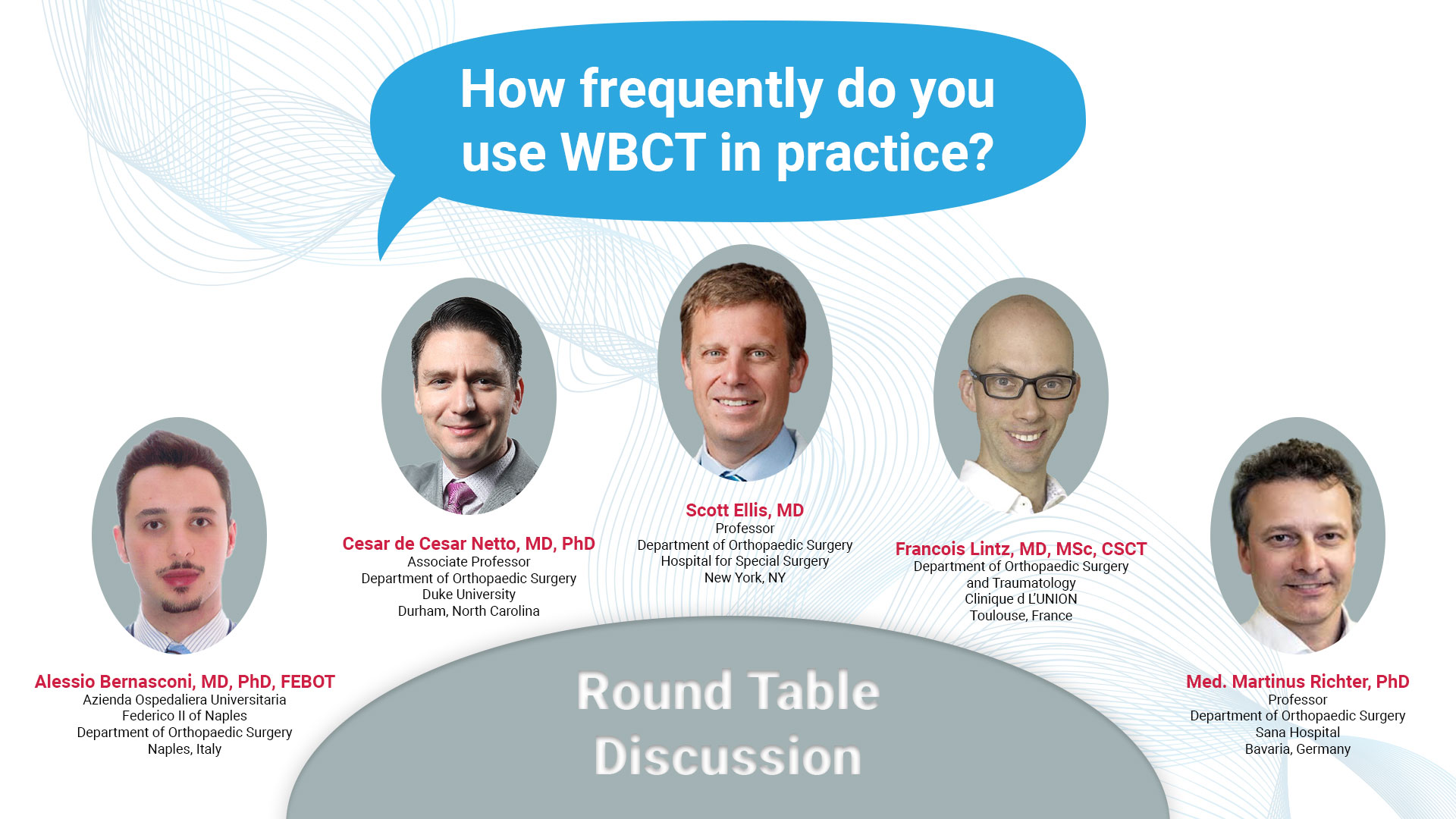
How Frequently Do You Use It In Practice?

Dr. Alessio Bernasconi, MD, PhD, FEBOT
Azienda Ospedaliera Universitaria
Federico II of Naples
Department of Orthopaedic Surgery
Naples, Italy
Unfortunately, at the university where I have recently been appointed, I don’t have a WBCT available yet. However, during 3 out of the last 7 years of my clinical practice I have had the chance to work in foot and ankle units where WBCT was on site and where I used to request scans regularly. Whenever bilateral standing radiographs would have been needed, a WBCT was performed instead. This was the case for diagnostic purposes but also for follow-up imaging at 3, 6 and 12 months after re-alignment procedures, fusions or arthroplasties.
I use WBCT every day. I order a WBCT scan before all my flatfoot reconstructions, fusions and hallux valgus procedures. I also obtain WBCT on all bunion surgeries about 3 to 4 months after surgery to assess healing and sesamoid/pronation correction. For the collapsing flatfoot, I regularly obtain WBCT imaging about 6 months after to assess healing of the correction. I learn a lot also from every case. For the Lisfranc and syndesmosis, I do not obtain it on every case. It is usually when I am trying to prove instability and the need for surgery. It might also help me fine tune plans for fracture fixation or midfoot fusion.

Dr. Scott Ellis, MD
Professor
Department of Orthopaedic Surgery
Hospital for Special Surgery
New York, NY

Dr. Francois Lintz, MD, MSc, CSCT
Department of Orthopaedic Surgery
and Traumatology
Clinique d L’UNION
Toulouse, France
That’s easy: I use it for every single patient. Every surgical patient will have it pre-operatively and at least once post-operatively. All other patients screened will have it as a primary modality. Cone beam CT, be it weight bearing or not, is equivalent to 3D radiography and that is where most of the healthcare benefits are for patients. It is also the most time and cost-efficient modality.
The reality is that if insurance was not an issue, I would not perform conventional radiographic imaging anymore. WBCT imaging allows superior and more complete 3-dimensional assessment of the foot and ankle, with low radiation dose. With available digitally reconstructed radiograph technology, if one would prefer, you can use 2D reformatted images rather the entire multiplanar reconstructions.

Dr. Cesar de Cesar Netto, MD, PhD
Associate Professor
Department of Orthopaedic Surgery
Duke University
Durham, North Carolina, USA

Med. Martinus Richter, PhD
Professor
Department of Orthopedic Surgery
Sana Hospital
Bavaria, Germany
More than 21,000 scans since 2013.
To read the full roundtable discussion visit https://journals.sagepub.com/doi/10.1177/19386400241238608