Orthopedic decision-making depends on accurate representation of anatomy—particularly when joint alignment and bone relationships change…
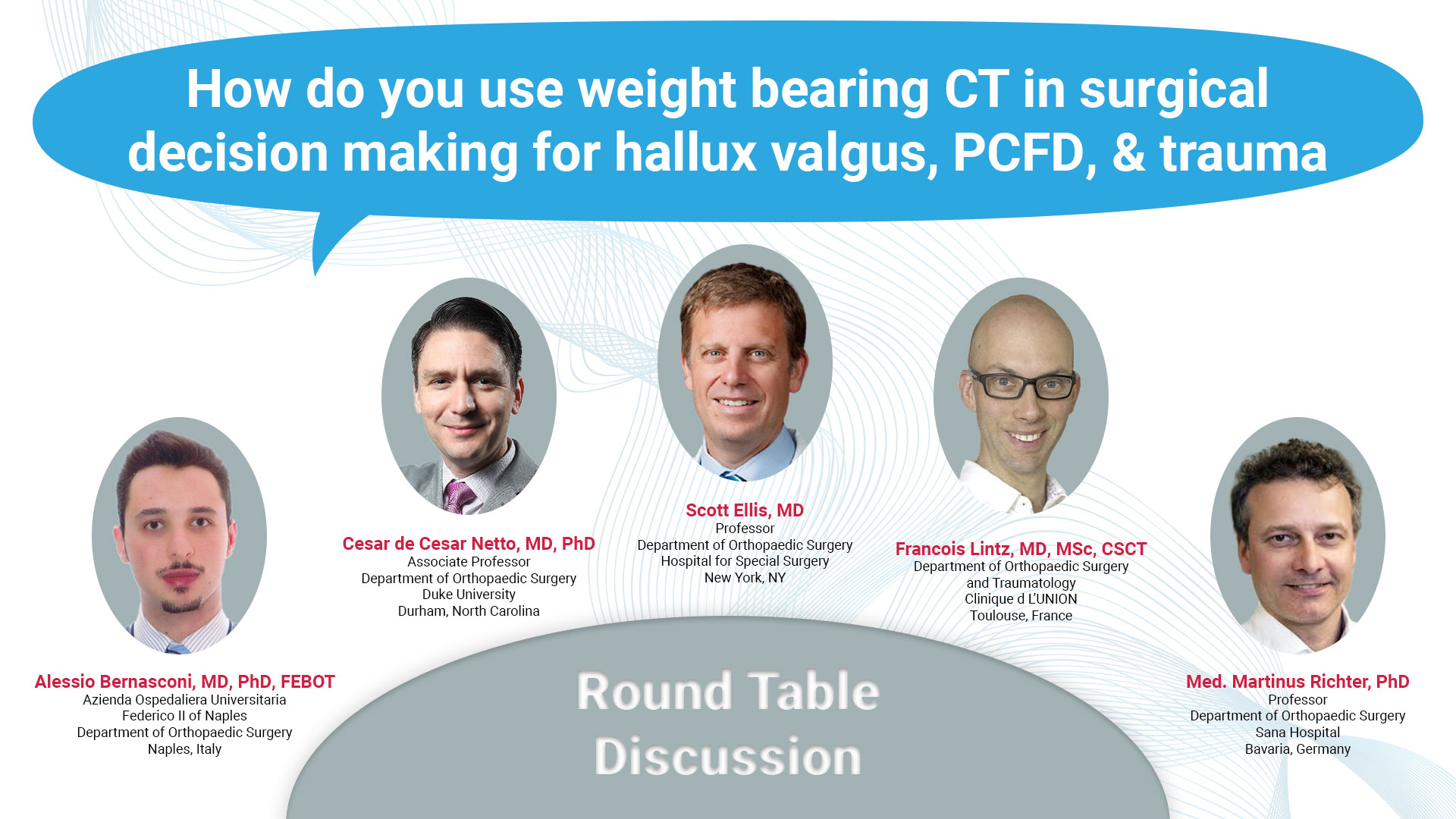
Surgeons Weigh In: Top Indications for WBCT Part 2
Weight bearing CT (WBCT) imaging has fundamentally changed the evaluation and management of foot and ankle disorders such as hallux valgus, progressive collapsing foot disorder (PCFD), ankle instability, and traumatic deformities. The following panelists of experts share their insights and experiences in the use of WBCT in clinical practice as well as the future direction of the modality.
How do you use it in surgical decision making for Hallux Valgus, PCFD, and Trauma (such as Lisfranc and Syndesmosis injuries)?

Dr. Alessio Bernasconi, MD, PhD, FEBOT
Azienda Ospedaliera Universitaria
Naples, Italy
Hallux Valgus: Getting a WBCT in this setting is crucial to assess the rotation and the torsion of the first metatarsal, the sesamoid malposition and the degree of osteoarthritis potentially already affecting the metatarsosesamoid joint. When performing distal metatarsal osteotomies (which I use very frequently in my practice), I often find it difficult to decide intraoperatively which is the final correct rotation of the metatarsal head. Even the push-off test (simulating load under the forefoot) is not always very accurate. That is why I particularly value the possibility to decide pre-operatively on WBCT scans how much the metatarsosesamoid complex should be de-rotated in order to avoid hypo or hypercorrection. I also like the fact that it’s easier to demonstrate a tarsometatarsal instability (plantar opening of the first TMT joint) which is of course suggested by clinical examination, but I think should also be quantified for medico-legal reasons.
PCFD: this probably best represents how WBCT is a game changer in complex three-dimensional foot and ankle deformities. In PCFD, WBCT is the only way to evaluate malalignment in three planes, to assess changes in the joint space under loading and to unmask PCFD-specific features such as the talocalcaneal impingement and the calcaneofibular impingement. In practical terms, WBCT helps 1) to decide whether a joint can be spared or not (using an extra-articular re-alignment procedure or a fusion, respectively) and 2) to gauge the real correction you want to achieve in order to restore a correct alignment of the whole foot (especially for combined osteotomies).
Trauma: In these injuries one would normally go for a standard radiography followed by second-line imaging such as CT. WBCT allows you to get all in one and bilaterally (although I am aware that not all the available machines on the market allow a simultaneous bilateral scan). In Lisfranc, WBCT enables to appreciate associated lesions such as small fractures of the metatarsals or bony avulsions which may guide your treatment. For syndesmotic injuries, while I acknowledge that in acute setting patients may sometimes be too uncomfortable to weightbear, it is important to try if possible. There is great value in comparing both ankles to reduce the chance of diagnostic error related to the large anatomical variability of the distal tibiofibular area. Overall, I see great value for WBCT in detecting “subtle” ligamentous injuries, which are those more likely to go unseen on traditional imaging.
Hallux Valgus: WBCT imaging is extremely helpful in the decision making of the surgical treatment options for hallux valgus deformity. I believe it’s paramount to assess the presence of mild but objective signs of medial column instability, with plantar flexion collapse of the navicular cuneiform joint, or plantar gapping of the first tarsometatarsal joint for example, evaluation of the rotational deformity of the first ray and 1st metatarsal, titration of the amount of sesamoid subluxation, assessment of the severity of any arthritic findings between the first metatarsal head and the proximal phalanx as well as the sesamoids, presence of signs of PCFD, that are not infrequent, as well as the assessment of potential lesser metatarsal adductus deformity.
PCFD: I think the literature for the use of weight bearing CT in progressive collapsing foot deformity is so extensive, that utilizing WBCT imaging is pretty much mandatory if you have access to it. It does help me to look for signs of high risk for progressive deformity such as a considerably inclined posterior facet of the subtalar joint in valgus, direct and indirect signs of sinus tarsi and sub fibular impingement, subtalar joint subluxation in the middle facet, as well as the assessment of the overall 3-dimensional deformity by utilizing the measurement foot and ankle offset (FAO). The combination of the assessment of these variables, allow me to provide my full assessment of the patient’s problem, the likelihood of progressive collapse, the potential success rate for conservative treatment, as well As for planning surgical treatment. If the patients are considerably symptomatic and already have several red flags for PCFD, I usually recommend surgery if they fail conservative treatment, and utilize findings such as the presence of sub fibular impingement to recommend a subtalar joint fusion for example.
Trauma: WBCT imaging is my preferred imaging modality as well for ankle sprain, foot sprain, as well as any possible associated fractures. There is enough data demonstrating considerably improved assessment of mild syndesmotic instability using WBCT imaging, as well as mildly frank instability. I also believe, that soon, WBCT imaging will allow us to understand much better subtle ankle instabilities in the setting of “benign ankle sprains,” demonstrating potential subtle malpositioning in the ankle mortise, particularly rotational malpositioning of the talus secondary to ligamentous instability.

Dr. Cesar de Cesar Netto, MD, PhD
Associate Professor Duke University
Durham, North Carolina

Dr. Scott Ellis, MD
Professor Hospital for Special Surgery
New York, NY
Hallux Valgus: I find it very helpful to assess the amount of first metatarsal pronation present as part of the hallux valgus deformity along with sesamoid arthritis and position. The anatomy of the first tarsometatarsal joint also can help me plan my cuts when I perform a Lapidus. I use this information to decide how much to rotate the metatarsal at the time of surgery and how I may need to release the lateral tissue or tighten the medial capsule to reduce the sesamoids.
PCFD: The WBCT gives me very useful information to direct surgical treatment in the setting of a collapsing flatfoot. First, I can assess where deformity occurs along the medial arch. Depending on the apex of the collapse, I decide on whether to perform a Cotton osteotomy, Lapidus, or even naviculocuneiform fusion. Markers of significant subtalar impingement at the angle of Gisanne or subfibular impingement often may lead me to perform a subtalar fusion.
Trauma: For the Lisfranc, I obtain comparison WBCT to see if widening between the first and second metatarsal bases is asymmetric and significant enough to warrant surgery. I can also assess intercuneiform instability which might require addressing this joint as well as any other avulsion or fracture fragments present elsewhere. For the syndesmosis, again the comparison study is very helpful. I can look at syndesmotic widening which might drive surgical treatment. Based on the literature, we can use syndesmotic volume also to assess diastases in the weightbearing position. This typically presents more challenges but is a very useful concept in my experience.
Hallux Valgus: WBCT has proven indispensable to me in all cases of 1st TMTJ instability and/or arthritis, enabling quantification of the pathological process using advanced tools such as distance mapping, and planning of surgical correction. However, most of the focus has for now been in assessing 1st ray pronation, in the first metatarsal as well as the sesamoid complex. For me the successful reduction during surgical correction is key to obtaining longstanding stability and pain-free patients. WBCT is also very important in evaluating lesser toe deformities, particularly the existence of subluxation of lesser MTP joints.
PCFD: WBCT has unveiled new ways to direct surgical treatment. The new PCFD classification cites useful tools such as the Foot Ankle Offset, and subluxation of the middle subtalar facet, as well as sinus tarsi impingement. I use the Foot Ankle Offset to let me know when conservative treatment is possible. If the talus centerpoint projects into the foot tripod or just on the edge, I know that insoles and rehabilitation may at least temporarily mitigate the collapse. If its way outside, surgery is inevitable. Middle facet subluxation and sinus tarsi impingement usually tell me a posterior subtalar fusion is mandatory. Finally, I can see clearly where the collapse is taking place on the medial column, which helps determine what associated procedures will be useful, such as cotton or TMT fusion.
Trauma: All foot and ankle traumas are complex due to the inherent anatomy of the foot, with 28 superimposed bones. The possibility of inaccurate or missed diagnoses ranging on average from 20 to 40% in the literature is impossible to ignore and warrants 3D imaging as a primary modality. The largely published benefits of WBCT in syndesmotic and Lisfranc traumas are in fact a niche and contribute only marginally to the vast improvement of healthcare that would result in implementing CONEBEAM CT (not immediately WBCT) as the primary modality in trauma instead of the old, costly, time and radiation-inefficient sequence of radiographs + MDCT. Nevertheless, I do use WBCT is trauma as well and find also that comparative distance mapping is the most efficient way to identify Lisfranc and syndesmotic instability. The only indications in emergency where I still ask for a conventional CT are polytrauma cases where soft tissue injuries may be associated and possible cases of infection or soft tissue tumors.

Dr. Francois Lintz, MD, MSc, CSCT
Clinique d L’UNION
Toulouse, France

Med. Martinus Richter, PhD
Professor Sana Hospital
Bavaria, Germany
I use it for analysis of deformity with angle measurement by hand or automatically as well as analysis of joint degeneration.
To read the full round table discussion visit https://journals.sagepub.com/doi/10.1177/19386400241238608