Orthopedic decision-making depends on accurate representation of anatomy—particularly when joint alignment and bone relationships change…
WBCT Better Detects Complexities of Flatfoot
Key Points:
- Weight Bearing CT (WBCT) imaging has facilitated the introduction of a new classification system for Progressive Collapsing Foot Deformity (PCFD), commonly known as flatfoot.
- WBCT is particularly useful in recognizing peritalar subluxation (PTS) components and impingements, which allows for better diagnosis of PCFD.
Flatfoot is a condition that affects the arch structure and alignment of the foot. How flatfoot is understood and classified has evolved over time. A brief history:
- In 1989, medical experts proposed a 3-stage classification system for adult acquired flatfoot associated with the dysfunction and ultimate rupture of the posterior tibial tendon (PTT).
- In 1997 a fourth stage was formally added: fixed rigid valgus deformity associated with arthritis of the ankle requiring a tibiotalocalcaneal (TTC) arthrodesis.
- In 2007 the fourth stage was divided in a revised classification as stage IV-A associated with supple tibiotalar valgus and stage IV-B associated with rigid deformities.
- In 2020, a group of experts proposed a new term for flatfoot: Progressive Collapsing Flatfoot Deformity (PCFD), as well as a new classification system. The new classification system divides deformities into two classes, rigid (stage 1) and flexible (stage 2) and includes all possible presentations in a PFCD patient: hindfoot valgus (class A), midfoot abduction (class B), forefoot varus/medial column instability (class C), peritalar subluxation (class D), and valgus of the ankle (class E). A key aspect of this newest classification system is that it is based on measurements made on weight bearing CT (WBCT) rather than conventional radiographs (X-Ray). WBCT is highly effective in recognizing PTS components and impingements, making it a valuable tool in diagnosing PCFD.
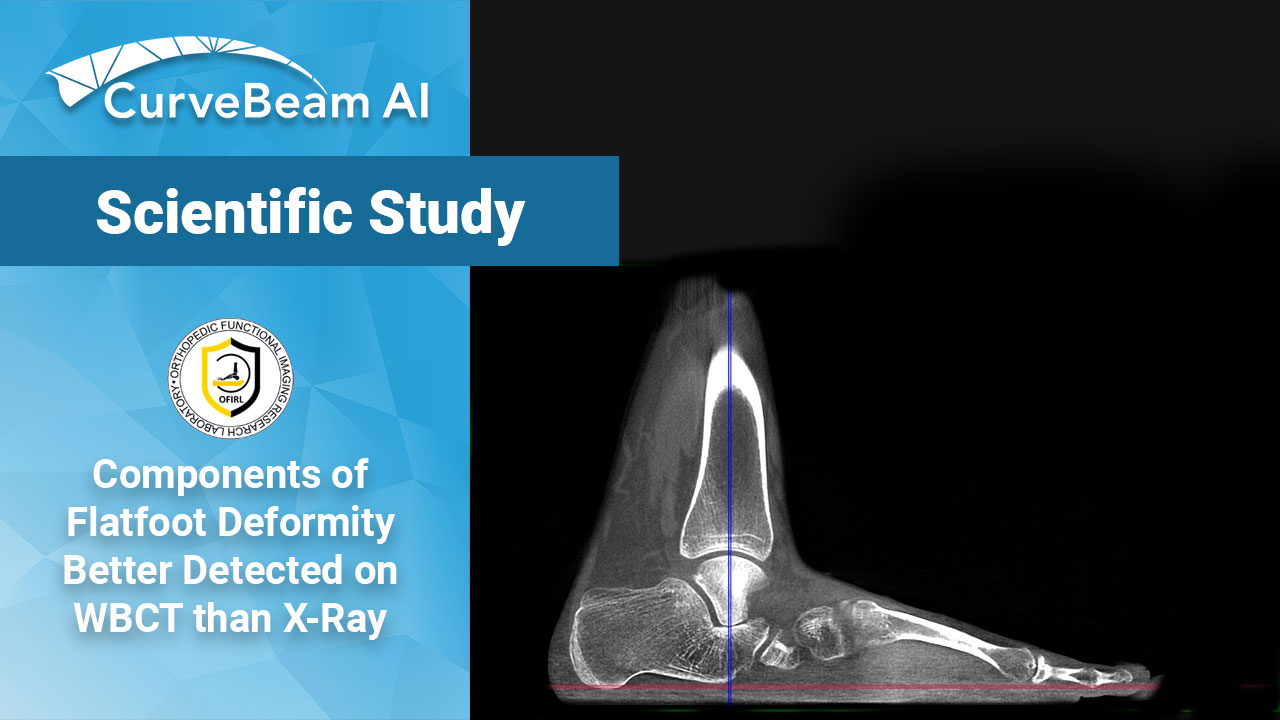
A recently published study, led by Dr. Cesar de Cesar Netto, aimed to compare how PCFD diagnosis would differ in patients if measured on X-Ray vs. WBCT.
The study was a retrospective comparison of 89 adult PCFD patients with no history of prior surgery or neuropathy, who were all evaluated clinically, with X-Ray and with WBCT imaging (CurveBeam AI’s pedCAT).
The results showed that when single components of PCFD were taken into consideration, a higher frequency of class B (89.9% vs 76.4%), class C (93.6% vs 86.2%), and class D (46.4% vs 34.8%) were noted when using the WBCT in comparison to CR, respectively. However, class A (83.9% vs 89.5%) and class E (27.7% vs 22.5%) had similar occurrences between the two methods.
The study found that the use of WBCT improved the overall accuracy and reliability of the PCFD consensus classifications. The modality was particularly useful in recognizing PTS components and impingement. The authors said WBCT could improve the diagnosis and treatment of PCFD, potentially leading to better outcomes.
To read the full article click here.