Read the article.
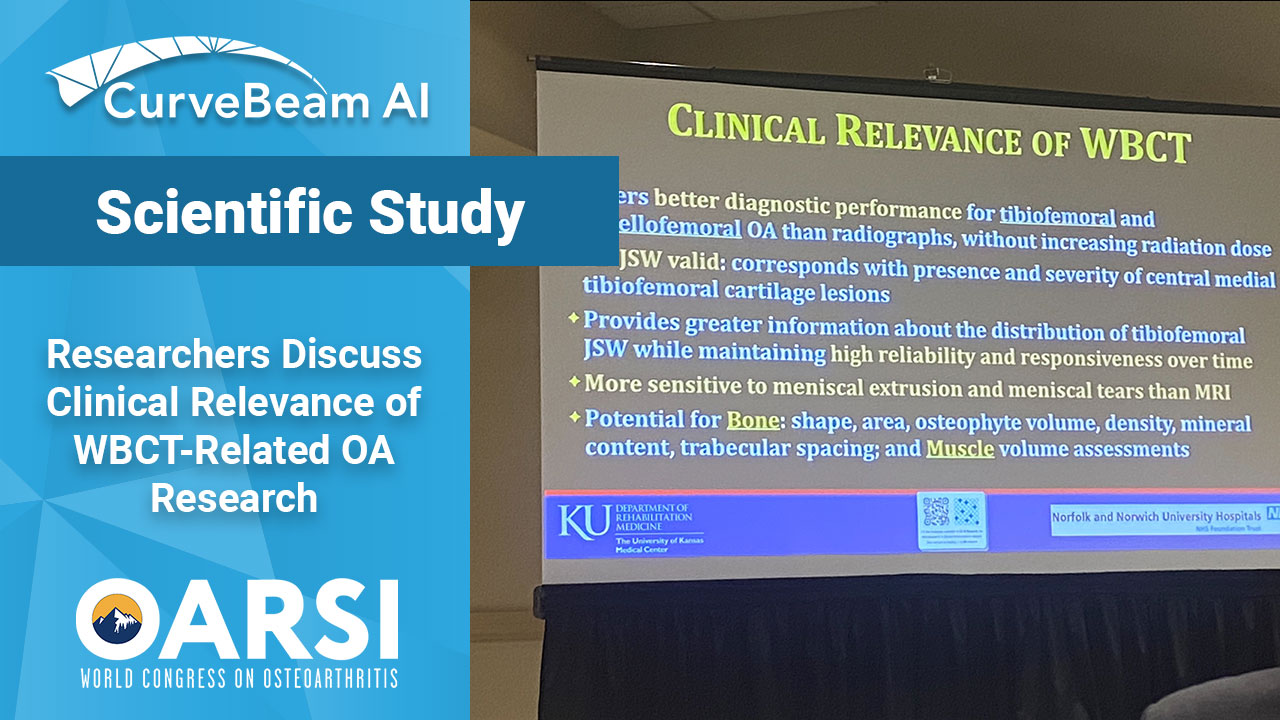
Researchers Discuss Clinical Relevance of Knee OA Clinical Trials Using WBCT
Knee osteoarthritis (OA) clinical trials results show that weight bearing CT (WBCT) imaging may offer new insights into OA pathology beyond what plain radiographs and MRI can provide. Some of these findings could immediately be translated into clinical practice as well.
Leading researchers presented these updates in a workshop titled, “Where Are We With Weight Bearing CT in OA Research and Do We Need it at All?” at the Osteoarthritis Research Society International (OARSI) World Congress on Osteoarthritis on Monday, March 20, 2023, in Denver.
One finding of clinical relevance is that WBCT arthrography (WBCTa) can detect meniscal tears and meniscal extrusions not seen on MRI, In one study (not yet published), WBCT detected extrusion not detected on MRI in 27.1% of medial and 8.5% of lateral menisci, and higher grades of extrusion for 30.6% of medial and 8.8% of lateral menisci.
The knees with greater medial and lateral extrusions on WBCT were predominantly in early stages of osteoarthritis. The Kellgren Lawrence grade was less than 2 for 80.5% of knees with medial extrusions and for 64% of knees with lateral meniscal extrusions.
A surgical validation study of these radiological findings is currently underway at The University of Kansas. This finding has, “changed clinical care where I am based,” said Dr. Neil Segal, MD, MS, who oversees the clinical osteoarthritis research program (CORP) at the University of Kansas Medical Center. “Regarding clinical care, our surgeons have altered surgical decisions based upon the results of WBCTa scans that we have done. For example, a meniscal root tear was detected on WBCTa that was not evident on MRI and explained the patient’s knee instability and severe pain, so she went for surgery that was indicated based on WBCTa, but not on MRI.” he added as additional commentary after the presentation.
Potential advantages of WBCTa in the clinical setting include a better understanding of three-dimensional meniscal position, and overall improved detection of meniscal pathology, according to the workshop presentation. WBCTa may improve surgical selection and provide earlier therapeutic opportunities for patients in whom pathology may have been missed.
WBCTa could also be useful for “the large contingent of patients” that are contra-indicated for MRI, said Dr. Tom Turmezei, MPhil, MA, BMBCh, PhD, FRCR, a consultant radiologist at Norfolk and Norwich University Hospitals NHS Foundation Trust in Norfolk, UK.
Presenters highlighted additional areas where WBCT may be clinically relevant for OA patients:
- Offers better diagnostic performance for tibiofemoral and patellofemoral OA than radiographs, without increasing radiation dose.
- Demonstrates higher sensitivity and accuracy for detecting osteophytes and subchondral cysts in comparison to fixed flexion radiographs.
- CT arthrography is the gold-standard for visualizing cartilage lesions.