Read the article.
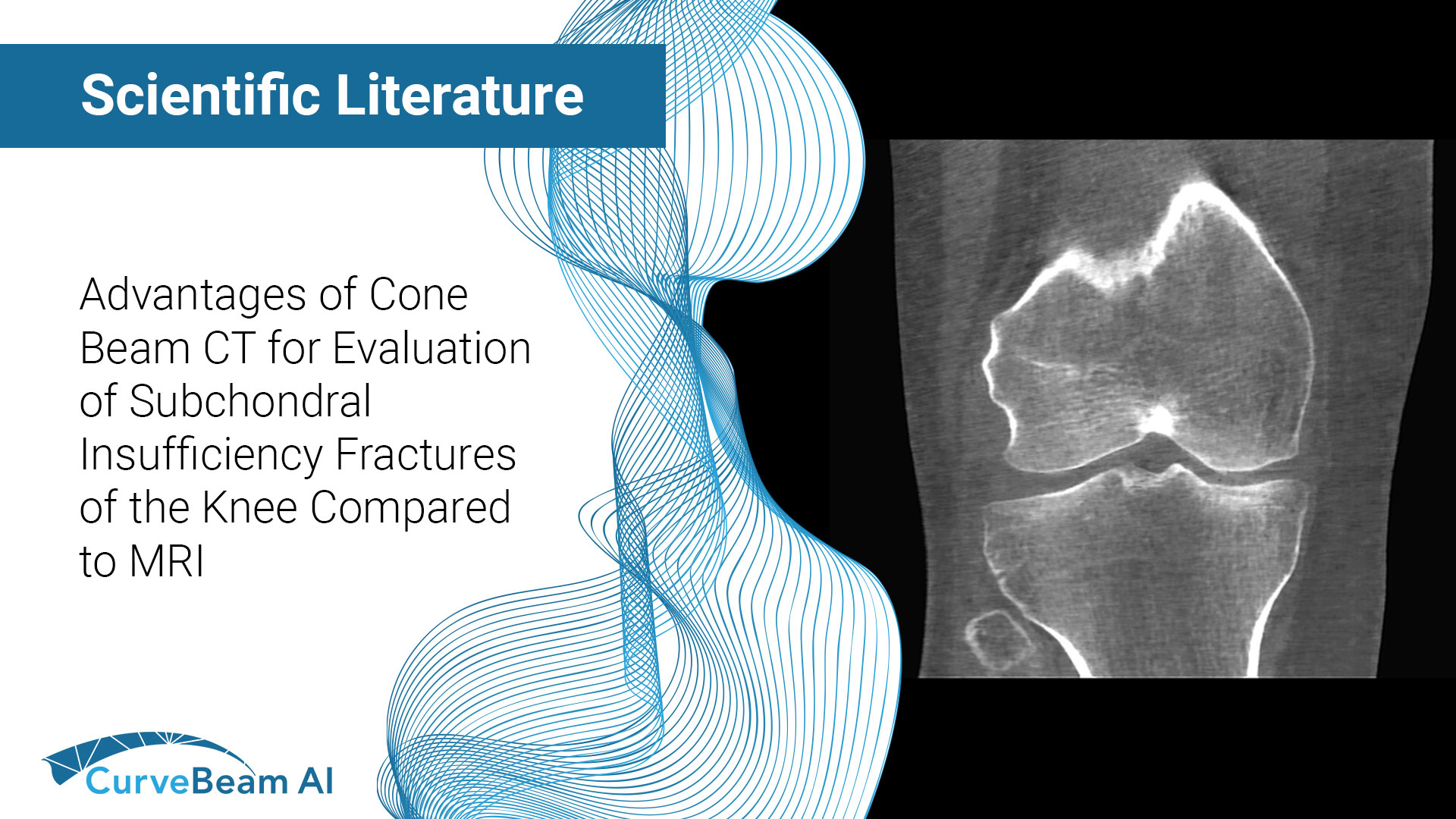
Advantages of Cone Beam Computed Tomography for Evaluation of Subchondral Insufficiency Fractures of the Knee Compared to MRI
Key Points:
- Cone Beam CT (CBCT) is superior in assessing bony structures compared to magnetic resonance imaging (MRI)
- In this study, there was a 40% rate of discrepancy when grading knee subchondral insufficiency fractures on CBCT vs. MRI, with MRI frequently underestimating damage of the subchondral bone plate while overestimating lesion size.
- CBCT is the imaging modality of choice for grading lesions and assessing subchondral bone plate integrity in the knee
Subchondral insufficiency fracture of the knee, also known as spontaneous osteonecrosis of the knee (SONK), is a musculoskeletal condition that usually presents clinically as atraumatic, sudden, non-specific knee pain accompanied by bone marrow edema (BME). This lesion typically occurs in the medial femoral condyle and is most common in patients older than 50.
While the current research in literature varies, it is believed that subchondral insufficiency fractures develop from BME with an increased risk of osseous lesions and subchondral bone plate instability along progression. In turn, they are a well-known factor contributing to the development of knee osteoarthritis (OA).
The continuity of the subchondral bone plate is important for defining the optimal treatment plan. Intact subchondral bone plate allows for a conservative treatment (reduced weight bearing, optimized supplements, and therapy), whereas in a case of collapsed subchondral bone plate, surgical evaluation is usually recommended (subchondral core decompression, osteochondral grafting, autologous chondrocyte implantation or even total-/uni-compartmental knee arthroplasty).
MRI is the current gold standard for subchondral insufficiency fracture grading and osseous defect size evaluation, with medical CT (MDCT) also being used preferably for subchondral insufficiency fracture evaluation and therapeutic decision-making. Proton density (PD) MRI sequences provide a high diagnostic accuracy in detecting early stages of lesions such as BME without osseous defects and T1-weighted sequences allow a detection of osseous lesions, though are less accurate than computed tomography (CT).
CBCT is a promising imaging technique that uses a three-dimensional (3D) conical X-Ray beam in combination with a flat panel detector. This method provides higher sensitivity and specificity in detecting fractures compared to X-Ray, as well as higher spatial resolution and lower radiation exposure than MDCT.
Dr. Maximilian M. Delsmann et al out of the Department of Osteology and Biomechanics, University Medical Center Hamburg-Eppendorf, Lottestraße, Hamburg, Germany aimed to investigate the diagnostic yield of CBCT in comparison with a 3 T MRI in the evaluation of subchondral insufficiency fractures of the femoral condyle in this retrospective study.
Defining the Study & Results
Researchers retrospectively analyzed 30 consecutive patients who presented at their outpatient clinic with new-onset atraumatic knee pain and no history of OA. MRI had been performed prior to presentation, showing femoral BME with suspected subchondral insufficiency fracture. CBCT of the knee was then performed to additionally evaluate the integrity of the subchondral bone plate to derive recommendations for conservative vs. surgical treatment options. In all patients, the time interval between MRI and CBCT was no longer than three months. Patients were then split into 3 grades and ratings were repeated after six weeks to determine reliability based on the following:
- Grade 1: no signs of subchondral bone lesion
- Grade 2: subchondral trabecular fracture or cystic changes, but without infraction of the subchondral bone plate
- Grade 3: collapse of the subchondral bone plate
Results showed that a considerable amount of cases exhibited a discrepancy between the gradings based on MRI and CBCT. More specifically, nine patients (30%) were diagnosed with higher lesion gradings in CBCT, whereas three patients (10%) presented a milder grading. It was noted the most frequent reason for the discrepancy was the interpretation of the subchondral bone plate integrity (10/12 patients; 83.3%).
Conclusion
Researchers concluded that comparison of MRI and CBCT revealed discrepancies in 40% of cases, with CBCT offering advantages in lesion characterization and MRI frequently underestimating damage of the subchondral bone plate while overestimating lesion size.
It was also noted that MRI appeared to be inferior in assessing bony structures compared to CBCT due to the uniform BME pattern in PD and even in T1 sequences, though MRI was superior to CBCT in the assessment of early stages.
To read the full study click here.